
Retina Services at Advanced Eye Care
- Macular Degeneration
- Macular Degeneration Treatment
- Diabetic Retinopathy
- Diabetic Retinopathy Treatment
Macular Degeneration
What is Macular Degeneration?
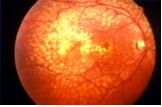
 Macular degeneration is an age-related condition of the macula, an area of the retina at the back of the eye that is responsible for seeing fine detail when reading or looking straight ahead. Macular Degeneration, often called AMD or ARMD (age-related macular degeneration), is the leading cause of vision loss and blindness in Americans aged 65 and older. Because older people represent an increasingly larger percentage of the general population, vision loss from macular degeneration is a growing problem.
Macular degeneration is an age-related condition of the macula, an area of the retina at the back of the eye that is responsible for seeing fine detail when reading or looking straight ahead. Macular Degeneration, often called AMD or ARMD (age-related macular degeneration), is the leading cause of vision loss and blindness in Americans aged 65 and older. Because older people represent an increasingly larger percentage of the general population, vision loss from macular degeneration is a growing problem.
Macular degeneration is diagnosed as either dry (non-neovascular) or wet (neovascular). Neovascular refers to growth of new blood vessels in an area, such as the macula, where they are not supposed to be. The dry form is more common than the wet, with about 85-90 percent of AMD patients diagnosed with dry AMD. The wet form of the disease usually leads to more serious vision loss.
Dry Macular Degeneration (non-neovascular). Dry AMD is an early stage of the disease and may result from the aging and thinning of macular tissues, depositing of pigment in the macula or a combination of the two processes.
Dry macular degeneration is diagnosed when yellowish spots known as drusen begin to accumulate from deposits or debris from deteriorating tissue mostly around the macula. Gradual central vision loss may occur with dry macular degeneration but is not nearly as severe as wet AMD symptoms.
There is ongoing research and trials available for treating dry macular degeneration. A major National Eye Institute study (AREDS) has produced strong evidence that certain nutrients such as beta carotene (vitamin A) and vitamins C and E may help prevent or slow progression of dry macular degeneration.
Dr. Stanciu also recommends that dry AMD patients wear sunglasses with UV protection against potentially harmful effects of the sun.
Wet Macular Degeneration (neovascular). In about 10 percent of cases, dry AMD progresses to the more advanced and damaging form of the eye disease. With wet macular degeneration, new blood vessels grow (neovascularization) beneath the retina and leak blood and fluid. This leakage causes permanent damage to light-sensitive retinal cells, which die off and create blind spots in central vision.
Neovascularization, the underlying process causing wet AMD and abnormal blood vessel growth, is the body's misguided way of attempting to create a new network of blood vessels to supply more nutrients and oxygen to the eye's retina. Instead, the process creates scarring, leading to sometimes severe central vision loss.
 What are the symptoms of Macular Degeneration?
What are the symptoms of Macular Degeneration?
There is no pain associated with dry or wet AMD. The most common symptom of dry AMD is slightly blurred or fuzzy vision requiring greater illumination to see greater details. Also, an inability to recognize faces at a distance may develop.
As dry AMD progresses, a blurred spot develops in the center of vision. With time, the spot may get bigger and darker, reducing central vision. Often, when dry AMD is limited to one eye patients do not complain of visual changes because of the ability of the other healthy eye to see clearly, allowing for driving, reading, recognizing faces and seeing fine details.
Symptoms of wet AMD may be that straight lines, such as sentences on a page, appear wavy; rapid loss of central vision; and a blurred or blind spot in the center of vision.
How is Macular Degeneration diagnosed?
If Dr. Stanciu suspects a patient of having AMD, she may:
- Perform a visual acuity test to measure vision at a distance
- Perform a dilated pupil examination to see the inside of the eye with an ophthalmoscope to check for drusen (tiny yellow deposits on the retina which are the most common early signs of AMD)
- Ask you to look at an Amsler grid with a pattern of straight horizontal and vertical lines. To the person with AMD, the lines appear wavy, distorted or missing or a black spot may appear in the center of the grid.
- Perform a fluorescein angiography. During this test, a dye is injected into the arm and quickly travels throughout the blood system. Once the dye reaches the blood vessels in the back of the eye, photographs are taken of the eye. The dye allows the ophthalmologist to detect blood vessels that are abnormal and leaking dye.
- Order an OCT (Optical Coherence Tomography). This test uses light waves to make a picture of your retina, allowing Dr. Stanciu to see any abnormal blood vessel growth.
What types of treatments are available at Advanced Eye Care & Laser Center for Macular Degeneration patients?
In the early stages of macular degeneration, regular eye check-ups, attention to diet, and possibly nutritional supplements (such as vitamins A,C, E and beta-carotene, zinc, and copper), and in home monitoring of vision may be all that is recommended.
Patients with advanced dry macular degeneration should check the vision in each eye, one at a time, at least once a day. By staring at the central point on an Amsler grid, patients can help monitor their vision regularly and can detect distortions in vision. These distortions represent the earliest stages of wet macular degeneration.
Amsler Grid:
Follow these instructions:Wear your reading glasses and hold the Amsler grid at a normal reading distance Cover one eye.
Look at the center dot and keep looking at it at all times.
While looking directly at the center, notice that all the lines are straight and all the small squares are the same size.
If you should notice any changes on the grid such as distortion, blur, discoloration, or other abnormality, and it stays that way for a few days, see Dr. Stanciu promptly.
Test the other eye in the same manner.
Lucentis
LUCENTIS® (ranibizumab injection) is an FDA approved prescription medicine for the treatment of patients with wet age-related macular degeneration (AMD). LUCENTIS is a breakthrough treatment for wet AMD that can do more than just help you maintain your vision. With LUCENTIS, people with wet AMD may see their vision improve or keep the vision they have.Wet AMD occurs when abnormal blood vessels grow in the back of the eye. As the blood vessels grow, they can leak blood and fluid, which damage the macula. The macula—which is the center of your retina—plays a key role in your central vision. LUCENTIS® (ranibizumab injection) is designed to block abnormal blood vessel growth and leakage.
Along with the abnormal growth of blood vessels, certain proteins are thought to play a big part in causing wet AMD. LUCENTIS is a treatment that targets these proteins—preventing them from causing more damage and possibly even reversing their effects.
Avastin
Avastin also known as bevacizumab is a drug closely related to Lucentis is also shown to be highly effective and a far cheaper alternative for people who have little or no health insurance coverage.At Advanced Eye Care, Dr. Stanciu has treated thousands of patients with both types of Macular Degeneration..
Diabetic Retinopathy
 A person with diabetes is at risk for developing diabetic retinopathy among other ophthalmic disorders. Diabetic retinopathy is the leading cause of new cases of legal blindness among working-age Americans. The longer a person has diabetes, the greater their chance of developing diabetic retinopathy.
A person with diabetes is at risk for developing diabetic retinopathy among other ophthalmic disorders. Diabetic retinopathy is the leading cause of new cases of legal blindness among working-age Americans. The longer a person has diabetes, the greater their chance of developing diabetic retinopathy.
In diabetic retinopathy the blood vessels of the retina become abnormal which may cause problems with eyesight. Normally, the blood vessels in the retina do not leak. In diabetic retinopathy, the retinal blood vessels develop tiny leaks. These leaks cause fluid or blood to seep into the retina. When the leakage accumulates in the macula, the macula becomes wet and swollen and cannot work properly. This is called macular edema and central vision becomes blurred. The form of diabetic retinopathy caused by leakage of the retinal blood vessels is called nonproliferative diabetic retinopathy (NPDR).
Another problem with the retinal blood vessels in diabetes is that they can become obstructed. The retinal tissue, which depends on those vessels for nutrition, will no longer work properly. The areas of the retina in which blood vessels have become obstructed then foster the growth and proliferation of abnormal new blood vessels, called neovascularization. Neovascularization can cause bleeding and scar tissue that may result in severe loss of vision or blindness. The form of diabetic retinopathy in which neovascularization develops (proliferates) is called proliferative diabetic retinopathy (PDR)
What are the symptoms of diabetic retinopathy?
G enerally, people with mild NPDR do not have any vision loss. A dilated exam is the only way to detect change inside the eye before loss of vision begins.
People with PDR experience a broader range of symptoms. They include:
- Dark floaters
- Loss of central or peripheral vision
- Visual distortions or blurriness
- Temporary or permanent vision loss
How is diabetic retinopathy diagnosed?
Diabetic retinopathy is diagnosed by dilating the pupil and looking inside the eye with an ophthalmoscope. If Dr. Stanciu discovers diabetic retinopathy, she may wish to order color photographs of the retina through a test called fluorescein angiography. During this test, a dye is injected into the arm and quickly travels throughout the blood system. Once the dye reaches the blood vessels of the retina, a photograph is taken of the eye. The dye allows Dr. Stanciu to detect damaged blood vessels that are leaking dye.It is important for patients to be aware of how well they are seeing with each eye. One way to test vision in order to detect even small changes when they first appear is to use the Amsler Grid.
Can diabetic retinopathy be prevented?
The most effective overall strategy for diabetic retinopathy is to prevent it as much as possible. Strict control of blood sugar levels will significantly reduce the long-term loss of vision from retinopathy. With improved diagnosis and treatment, only a small percentage of people with retinopathy develop serious vision problems.
How is diabetic retinopathy treated?
Laser surgery can be very helpful for the treatment of diabetic retinopathy. The laser beam is a high energy light that turns to heat when it is focused on the parts of the retina to be treated; this is called photocoagulation. In nonproliferative diabetic retinopathy (NPDR), the laser heat either seals the leaking blood vessels of the macula or reduces their leakage and allows the macula to dry. In proliferative diabetic retinopathy (PDR), the laser destroys the diseased portions of the retina. This causes the neovascularization to stop growing, become inactive and, in some cases, disappear.The major purpose of laser surgery is to prevent further visual loss. Laser surgery may not always be necessary and, in some cases, may not be possible because the degree or severity of the diabetic retinopathy may be too great. The decision to use laser depends mostly on the type of diabetic retinopathy, its severity, and Dr. Stanciu’s judgement regarding how well it may respond to laser surgery. Even following surgery patients continue to lose vision and require either further laser surgery or vitreous surgery.
People with diabetes should have an eye examination at least once a year. More frequent exams may be necessary after diabetic retinopathy is diagnosed.


